
You’re aging. You’re a woman. You have a diet low in calcium.
Those and other factors mean you could be at higher risk for osteoporosis, a medical condition in which bones become weak and brittle and more susceptible to fracture.
Osteoporosis, which affects more women than men, has a variety of causes. Certain medical conditions such as thyroid disease can lead to osteoporosis, as well as long-term use of medications such as steroids. The loss of estrogen during menopause may also be a contributing factor. If you don’t get much calcium, are sedentary and use tobacco and alcohol, osteoporosis can develop. Genetics may play a role as well, as individuals who have family members diagnosed with osteoporosis may be at risk themselves.
Osteoporosis is more common in Caucasian and Asian women, but women (and men) of all races are vulnerable.
Many of us don’t realize it, but bones are living tissue and undergo a constant regenerative process. There is a balance between new bone that is grown each month and bone that is lost. As we age, the balance between the two is disrupted, resulting in a greater loss of bone than gain. The result may be osteoporosis.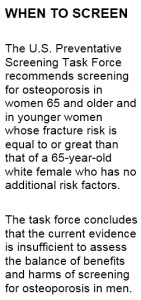
People who developed peak bone mass in their youth are much less likely to develop the condition. Symptoms of osteoporosis can include loss of height, back pain, stooped appearance, or a fracture that occurs easily.
People with osteoporosis are particularly vulnerable if they fall. Hip fractures greatly impact a person’s quality of life. An individual who fractures a hip has a 50 percent chance of never walking again without a cane or walker.
And here’s a sobering fact: One in five people who suffers a fracture lives less than one year post fracture. Even without falling, osteoporosis can cause fractures in the spinal bones that may cause back pain and lead to the “humped” over posture frequently seen in the elderly.
Although we can’t see our bones in the mirror, we can evaluate them. Ask your doctor or nurse practitioner if you should undergo a bone density screening. The screening is non-invasive, easy and safe to do and can identify early signs of bone loss.
If the test does identify bone loss, your provider may recommend lifestyle changes, such as increasing calcium and vitamin D in your diet, performing weight-bearing exercises (such as walking) each day, eliminating use of cigarettes and alcohol, or a medication regimen to help restore and maintain your bone mass. Bisphosphonates are medications that are widely prescribed for osteoporosis.
Here’s a look at some recent cases handled by JU nursing faculty and students:
ESTHER
Esther, 46, presented to an off-site clinic for her annual exam and was evaluated by a JU family nurse practitioner student and her faculty instructor.
Although Esther considered herself healthy and watched her diet, she had a long history of asthma and required steroids at times to control it. The student recommended Esther have a bone density screening. The result showed early signs of osteoporosis. Esther was advised to consume adequate amounts of calcium and vitamin D and to begin a walking regimen holding light hand weights.
Esther will return to the clinic in a year to repeat the bone density screening to reevaluate how well her bones respond to the treatment.
MARGARET
Margaret, 50, told the family nurse practitioner student that her older sister had recently fallen and suffered a hip fracture. Margaret was very conscientious about her health, ate well, exercised regularly, did not smoke, rarely consumed alcohol and had no other risk factors of osteoporosis. Despite her focus on prevention, Margaret’s bone density test showed osteoporosis. The student and her faculty instructor placed her on a medication to protect her bones. A repeat bone screening the following year showed an improvement in Margaret’s bone density. In this case, early identification helped preserve Margaret’s bone density and lessened her risk of fracture.
Nursed to Health is an occasional feature in which Jacksonville University School of Nursing faculty discuss symptoms, diagnoses and treatments based on composites of patient cases handled by instructors, students and alumni of JU’s local training programs. Today’s column is by Dr. Hilary Morgan, JU Assistant Professor of Nursing and a Certified Nurse Midwife and instructor in the Family Nurse Practitioner program. It appeared in The Florida Times-Union on April 29, 2015.
Information for Nursed to Health is based on actual and composite cases of patients treated by students, alumni and faculty of Jacksonville University’s School of Nursing. Names and specific medical information have been changed to protect private health information, and any similarity is coincidental. For more information about JU’s School of Nursing, visit www.ju.edu/chs. Readers with specific questions regarding their own health concerns should seek the advice of their healthcare provider.
 Wave Magazine Online Jacksonville University News Hub
Wave Magazine Online Jacksonville University News Hub
